[A guest blog from Wendy Perera, MBA, MSN, BSN, RN, PMGT-BC, NEA-BC, Alumnus CCRN Chief Nurse Executive ~ PereraHealth. Part 2 of a 3 part series on healthcare communication]
In our last blog “Communication Tools in Healthcare, do they improve your work environment?” We discussed healthcare team members’ concern for a lack of resources in communication tools. These tools are requested for team members to share what they need from their work environment, to ultimately be successful in their assigned roles, to feel safe themselves and to facilitate safe patient care.
High Reliability Organizations (HROs) also focus on achieving a culture of safety through transparency. Fostering a culture where we can learn from open discussion of observations, and near-misses, by not being afraid to openly share our observations and our suggested solutions. In this post, we’ll delve into what helps or hinders open sharing of workplace issues and how to promote a culture of safety for team members and patient safety.
Transparency defined
Transparency is “the quality of being done in an open way without secrets.” In the context of healthcare and HROs, we can say, for example, we need healthcare team members to be more transparent with their leaders about their day-to-day observations and experiences so we can improve upon processes and prevent safety concerns for co-workers and patients.
However, is being transparent confusing with actually being able to see an individual?
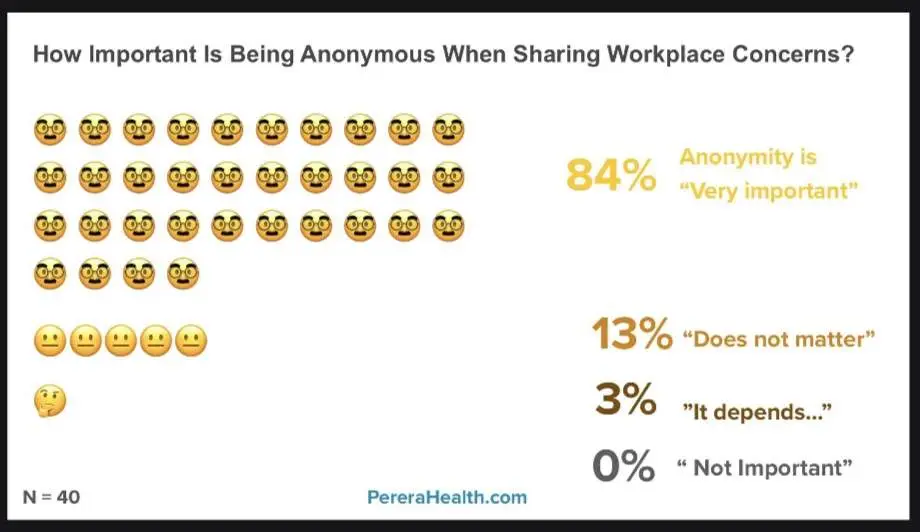
Healthcare team members are stating their organizations don’t always provide anonymous resources for sharing of information. Team members state they would like anonymous sharing for social safety. They want to do the right thing and share concerns but don’t want to risk being judged or getting in trouble with peers, other professionals (e.g., MDs, pharmacists) or even their leaders. In this circumstance, anonymity plays an important role in being fully “transparent.”
Defining Unintentional Silencing and Intentional Silencing and why it matters?
“Unintentional” signifies something not deliberate, inadvertent, or without deliberate intent. Therefore, “unintentional silencing” refers to silencing that occurs inadvertently or not by design.
In our previous blog, “Communication Tools in Healthcare,” we explored some communication tools within healthcare that might inadvertently lead to silencing some points of view.
In this blog we will continue to explore forms of “unintentional silencing” as well as “intentional silencing,” which involves deliberate and purposeful actions designed to control a situation or dialogue.
Healthcare’s History with Silence
Did our history of silence start with the Health Insurance Portability and Accountability Act (HIPAA) of 1996, or does it trace back to an earlier unwritten code of silence? HIPAA is both a law and a reminder that individual private information can only be shared on a need-to-know basis. Is the healthcare industry more inclined to maintain secrecy rather than promote open sharing, even when it could lead to improving outcomes in the future?
Sources of Healthcare Unintentional Silencing
Consider 1:1 team member rounds again, this time for service lines with larger teams, such as Emergency Room, Med-Surg, Critical Care, Sterile Processing, Surgical Services, and Interventional Procedural Suites. These departments operate around the clock, with leaders less frequently available during evenings, nights, weekends, and holidays. Even when leaders are present during these times, they may be fatigued from having worked an extended shift, further not being perceived as fully engaged. How are these teams communicating if not for emails or sticky notes?
What about compliance surveys? Have you ever received instructions via email or other communications on what to say and what not to say to surveyors? My first encounter with this was directly from a compliance surveyor consultant, not the hospital administration’s directive. We were coached by these consultants on how to navigate surveys without triggering additional scrutiny. Shouldn’t we strive to identify areas for improvement? Why was open transparency discouraged?
HRO safety huddles had many healthcare team members feeling this could replace the monthly staff meeting, but some organizations hold a strict 10 minutes or less conversation and are only allowed to share identified safety issues.
On-line meetings by Zoom, Google Meet, Teams, and other platforms boomed during the pandemic, but so did requests for healthcare leaders’ time. Anybody with your email, could place a meeting on your calendar and multiple at the same time. This mode of communication has pulled clinical leaders more into their offices and away from their teams.
Sources of Healthcare Intentional Silencing
Healthcare team members have long complained of issues of harassment and bullying, which constitute intentional forms of silencing. Despite the presence of experts dedicating their entire careers to addressing these issues, workplace incivility continues to be a concern. Recently, a nurse leader came across the concept of “workplace mobbing” or retaliation for speaking up, during an employee interview. The interviewee was asking about work culture in making a final determination on where to work.
Resources Are Being Requested
Over the past two decades, the Agency for Healthcare Research and Quality (AHRQ) through TeamSTEPPS® has been promoting the importance of healthcare team members speaking up for safer patient care. Since 2006, teams have been trained to utilize CUS: “I am Concerned,” “I am Uncomfortable,” and if needed, escalate to declare a “Safety issue” and “Stop the line.” However, AHRQ acknowledged that these tools were designed to enhance patient safety, not individual team member workplace concerns.
Recently AHRQ has introduced additional tools to help manage conflicts among coworkers at the moment they occur. They have introduced the “I’M SAFE” acronym, aimed at empowering newer generations of healthcare team members to speak up when they need a break, rest, or support from colleagues.
TeamSTEPPS® educators did indicate that team members who feel isolated or misunderstood are less likely to voice concerns.
In our cover image, direct care team members and leaders clearly expressed their need for an anonymous platform to share workplace concerns, with 85% stating anonymity was “very important.”
Conclusion
Empirical evidence strongly suggests communication tools for healthcare team members are lacking. Since healthcare organizations are responsible for providing resources for their team members to effectively do their jobs. They need to provide tools that foster open communication to let team members share their observations and experiences in a constructive manner that helps solve the issue by identifying solutions. This blog demonstrates that these tools should also be anonymous, and encourage transparency.
Yell’o™ is a new way for front line healthcare team members to anonymously post workplace issues and suggest solutions using a mobile phone… right at the moment they observe them…not a month later at some scheduled meeting.
- Be it broken equipment, Pyxis issues, supply concerns, run-of-the-mill compliance matters, or workplace suggestions
- Be it in a surgical suite, a restroom, ICU, ED, the Cath Lab, SPD, back hallway near the loading dock, or wherever
- Be it 2 o’clock in the afternoon on a Tuesday or 2:00am on a Saturday, even if it’s New Year’s Day
And it’s as simple as, but more advanced than, well, sticky notes… and way better than emails!
👉 Did we mention the issues and solutions are transported directly to the department that can fix them and NOT your over-burdened manager!?
Yell’o™ works to make healthier, safer, and happier workplaces.
If it improves the lives of those caring for your patients, it improves your patient care.
Additional Resources
Health Insurance Portability and Accountability Act (HIPAA) of 1996
Agency for Healthcare Research and Quality (AHRQ) TeamSTEPPS®3.0
High Reliability Organizations (HROs)
Could the absence of communication tools in use for healthcare team members be contributing to trust issues? Find out more in our next blog.
Author: Wendy Perera, MBA, MSN, BSN, RN, PMGT-BC, NEA-BC, Alumnus CCRN
Chief Nurse Executive ~ PereraHealth
Co-founder & CEO Yell’o™
Contact Info: [email protected]
https://pererahealth.com
Wendy @ http://linkedin.com/in/wendyaperera
Yello @ http://linkedin.com/in/phyello